Prenatal Genetic Testing
Genetic testing for pregnant women at a glance
- Two types of genetic testing are available to women who are currently pregnant, aneuploidy screening and carrier screening.
- Aneuploidy screening involves examining the current pregnancy for chromosomal abnormalities that will affect the fetus such as extra or missing chromosomes that may cause genetic disorders like Down syndrome or birth defects.
- The two methods for aneuploidy screening are amniocentesis or a combination of blood testing and ultrasound imaging.
- Carrier screening examines the parents to determine if they have any genetic disorders, such as cystic fibrosis or sickle cell anemia, that could be passed on to the fetus.
Do you have questions about genetic disorders or pregnancy? Let’s set up a time to discuss them.
Request Appointment
What is prenatal genetic testing?
Genetic, or inherited, anomalies can be passed from either mother or father to a fetus at the time of conception. One in 200 pregnancies involve genetic disorders and the likelihood that the pregnancy will result in a genetic disorder increases as women age. Genetic testing can help patients to identify potentially catastrophic abnormalities such as trisomy 13 or 18, and to inform them of life-changing genetic abnormalities like cystic fibrosis and Down syndrome.
Families can feel differently about genetic testing. At University of Colorado OB-GYN, we are here to help patients make the decision best for them and their family. Some women and couples want to know information about their baby to prepare themselves and their families. Others wish to know information and may choose not to continue the pregnancy based on the results.
Women who feel confident that genetic testing results would not change their mind about the pregnancy often choose to forgo all genetic testing. Choosing to do no testing is a perfectly valid option.
What is aneuploidy?
All humans have 23 pairs of chromosomes to produce 46 chromosomes in total. In humans, an extra chromosome can exist within 21 of the 23 pairs of chromosomes, resulting in what is known as a trisomy. We see this triplicate abnormality most commonly on chromosome 21, and this is called trisomy 21 or Down syndrome.
Other chromosomes can also have this triplicate abnormality but they are rarer like trisomy 18 and trisomy 13. Human sex chromosomes can also have triplicate chromosomes, for example an XXY presentation, as opposed to an XY, is known as Klinefelter syndrome.
It is also possible for a chromosome to be absent from a pair, resulting in what is known as monosomy. One instance is the absence of a sex chromosome resulting in an X0 as opposed to the usual XX gene presentation. This is known as Turner syndrome.
While all women are at risk for having a chromosome abnormality, women over age 35 have a high chance of giving birth to a child with a chromosomal abnormality, such as trisomy 21.
Currently, no therapies or interventions exist to change the chromosomes of fetus’ with trisomy.
Types of prenatal genetic abnormality testing & diagnosis
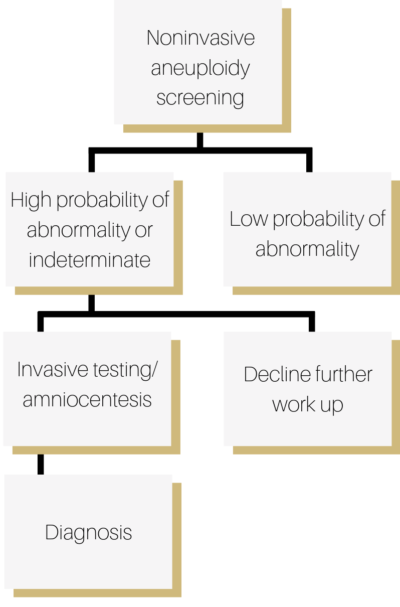
Patients interested in genetic testing and diagnosis have two procedural options: noninvasive and invasive. Doctors often begin with less invasive measures if an abnormality is suspected or identified during an ultrasound, starting with blood testing.
Noninvasive testing means that the pregnancy will not be harmed by the procedure. These tests are less accurate, but present no risk to the pregnancy. If testing returns with “low probability” of abnormality, then no further testing is recommended.
If the testing returns with “high probability” or an “indeterminate” result, then an invasive test may be recommended for definitive diagnosis. Invasive measures are those that could cause potential harm to the pregnancy such as amniocentesis, a procedure where a needle is placed through mom’s abdomen in order to extract fluid to be analyzed for genetic information.
Carrier screening for diseases like cystic fibrosis
Carrier screening means we test patients who are already pregnant or looking to conceive to see if they “carry” a genetic mutation. When both parents are healthy, we know they do not have a specific disease, like cystic fibrosis, but there could be some question as to whether they carry the disease. If both parents are “carriers” of a disease, they could each pass that abnormality to their children, resulting in children who have a hereditary disease.
How does carrier screening work?
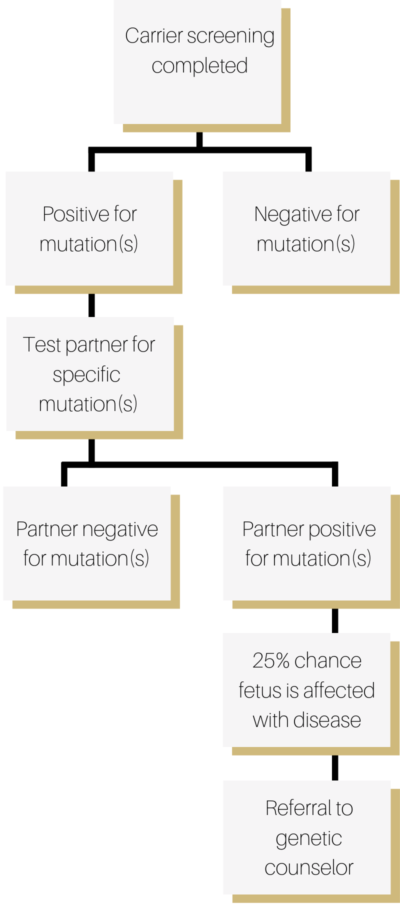
For interested couples, we first draw mom’s blood and test for abnormalities that she might carry. If she tests positive for any abnormalities, then we test dad for just those abnormalities. If she tests negative for any abnormalities, then we do not test the father.
Which genetic diseases can we test for?
Carrier screening is designed for “autosomal recessive” genes. This means both parents must have the abnormal gene for their child to be at risk. Examples of these genes include but are not limited to cystic fibrosis, sickle cell anemia, spinal muscular atrophy, and Tay-Sachs disease. Pregnancy care providers will often discuss and recommend tests that are most appropriate based on each partner’s ethnic background and health history.
Patients can opt to be screened for individual genes, or a panel (multiple genes). Keep in mind that the larger the panel, the higher the chance that a person will test positive for a mutation.
What to do after positive test results
The first step after a positive result is to test the other partner. If the other partner is negative, the likelihood that the fetus will be affected is very low.
If both partners test positive for a recessive gene, there is a 25% chance that the child will be affected with the disease. We recommend discussing the next steps with a genetic counselor, as the recommendations will vary based on the specific disease.
What about testing other genes like breast cancer (BRCA) or colon cancer (Lynch syndrome) genes?
These tests are reserved for patients with specific family history of breast or ovarian cancer. While the results may affect decisions around pregnancy, they are classified as “hereditary cancer genes,” not “prenatal genetic testing.” Patients interested in learning more should discuss their concerns with their provider.
How much does genetic testing cost?
Each insurance carrier has its own policy on prenatal genetic testing. We recommend patients call their insurance company to get an understanding of what is covered. The following codes and terms may be helpful to confirm coverage.
Aneuploidy screening
- Genetic ultrasound (Nuchal translucency) CPT code 76813.
- Sequential Integrated Screen Part 1 CPT code 81508.
- Sequential Integrated Screen Part 2 CPT code 81511.
- Cell free DNA testing CPT code 81420.
Carrier screening
- Cystic fibrosis screening CPT code 81220.
- Spinal muscular atrophy CPT code 83912.
- Sickle cell anemia CPT code 83021.
- Thalassemia anemia CPT code 83021.
- Tay-Sachs CPT code 81255.
